Living with PCOS can often feel like you’re trying to make sense of something that’s always changing. The uncertainty of not knowing what’s next or how to best manage this condition can be physically and emotionally draining. You might find yourself asking, “How do I take control of this?” and “Where do I even start?”
Your OBGYN can make a real difference. They’re more than just a healthcare provider; they’re your partner in understanding PCOS. In this blog, we’ll explore how a specialist can guide you, create a plan that fits your needs, and provide care that empowers you to manage PCOS.
What PCOS Is and Who It Affects Most
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects the functioning of the ovaries. This condition arises from a hormonal imbalance, including fluctuations in insulin and androgens, which can interfere with the usual processes of ovulation and fertility. While PCOS is a leading cause of infertility, its symptoms can vary widely, affecting different aspects of a woman’s health if not properly managed.
PCOS is often diagnosed in women during their reproductive years, with many cases identified in the late teens or early twenties. It is estimated that approximately one in ten women of childbearing age are affected by this condition.
However, the impact of PCOS is unique to each individual. The severity of symptoms, their manifestation, and the long-term effects can differ, making personalized care and management crucial for those living with PCOS.
How Your OBGYN Can Help Manage Symptoms
An OBGYN is a specialist trained in both obstetrics and gynecology, which means they handle everything from pregnancy and childbirth to the complexities of the female reproductive system. This combination of skills makes them the go-to expert for managing a variety of conditions, including Polycystic Ovary Syndrome (PCOS).
When it comes to PCOS, an OB gynecologist takes a well-rounded approach to your care. They understand that every woman’s experience is different, so they don’t just focus on the symptoms—they look at the bigger picture. By addressing both the hormonal and physical aspects of PCOS, they create personalized plans designed to fit your needs and goals.
More than anything, they’re a partner in your health journey. They’ll answer your questions, explain what’s happening in your body, and support you every step of the way. Managing PCOS might feel overwhelming, but with the guidance of a caring and knowledgeable OBGYN, it becomes much more manageable.
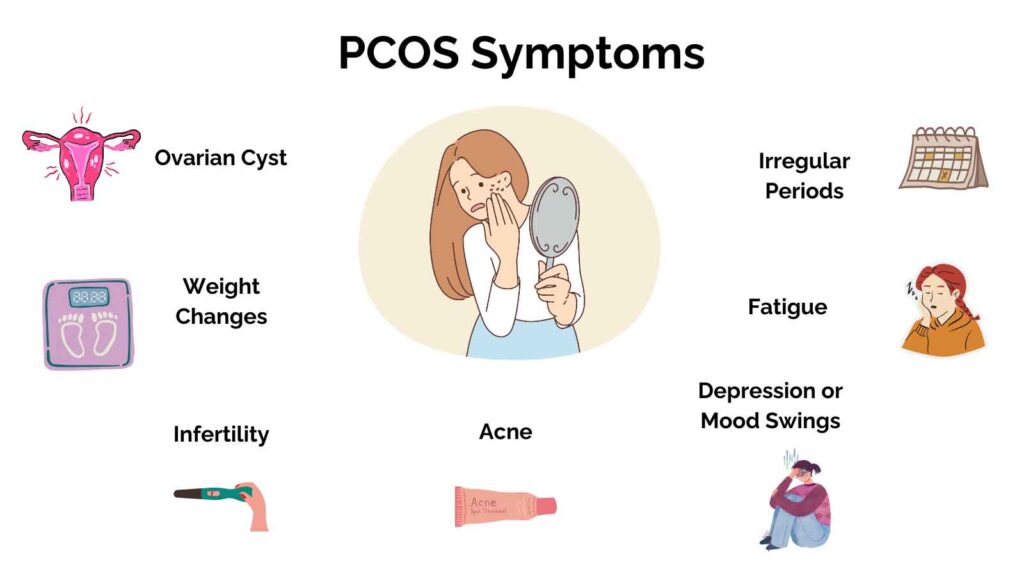
Here’s how your OBGYN can help manage some of the most common symptoms of PCOS:
- Ovarian Cysts: Women with PCOS often develop cysts on their ovaries due to the hormonal imbalances that prevent normal ovulation. While most cysts are benign and do not cause serious health issues, your doctor can monitor their size and help manage any discomfort. In some cases, medication or surgical options may be considered to prevent the cysts from growing or causing pain.
- Weight Changes: Many women with PCOS struggle with weight gain or difficulty losing weight due to insulin resistance. Your gynecologist doctor can guide you on nutritional choices and physical activity, in addition to prescribing medications to regulate insulin levels. In some cases, weight management strategies are critical not just for symptom relief but also to reduce the risk of developing other conditions like diabetes.
- Infertility: One of the more challenging aspects of PCOS is its impact on fertility. Because PCOS disrupts ovulation, it can make it harder for women to conceive. They can offer treatment options such as ovulation-stimulating medications or, if needed, assist with fertility treatments like in vitro fertilization (IVF) to help you achieve pregnancy.
- Acne: Elevated androgen levels in women with PCOS can lead to an increase in facial and body acne. Your OBGYN can prescribe medication, such as oral contraceptives or anti-androgen drugs like spironolactone, to help regulate hormone levels and reduce acne outbreaks.
- Depression or Mood Swings: Hormonal imbalances associated with PCOS can sometimes lead to mood swings, anxiety, or even depression. A gynecologist specialist can help identify these mood disturbances and recommend treatments, including counseling or medication, to address mental health alongside physical health.
- Fatigue: Many women with PCOS experience chronic fatigue due to hormonal fluctuations and sleep disturbances. An OBGYN can assess underlying causes such as insulin resistance, sleep apnea, or thyroid dysfunction, and suggest lifestyle changes or treatments to improve energy levels.
- Irregular Periods: One of the hallmark symptoms of PCOS is irregular or absent menstrual cycles. This is caused by hormonal imbalances that affect ovulation. These professionals can help regulate your periods through birth control methods, hormonal therapy, or other medications, providing relief and making it easier to track and manage your cycle.
How is PCOS diagnosed?
Diagnosing Polycystic Ovary Syndrome (PCOS) requires a comprehensive evaluation by a healthcare provider, typically an OBGYN. Since the symptoms of PCOS can vary widely and overlap with other conditions, a thorough diagnosis is essential for effective management. The process typically involves several key steps, including a detailed medical history, physical examination, and diagnostic tests.
- Medical History and Symptoms Review
The first step in diagnosing PCOS is a conversation with your healthcare provider about your symptoms and medical history. Gynecologists will ask about the onset and nature of your menstrual cycle, any changes in weight, acne, or hair growth, and whether you’ve experienced any fertility challenges. This helps your doctor identify patterns or signs that may suggest PCOS. - Physical Examination
Next, your OBGYN will perform a physical examination. This may involve checking for physical signs of PCOS, such as excessive hair growth (hirsutism) or acne. They will also assess your overall health, including your weight, blood pressure, and any signs of insulin resistance, which is commonly associated with PCOS. - Blood Tests
Blood tests are crucial to the diagnostic process. They measure hormone levels, including androgens (male hormones), insulin, and other key hormones that regulate the menstrual cycle. Elevated androgen levels, in particular, can indicate PCOS. Blood tests can also help rule out other conditions that might mimic PCOS, such as thyroid disorders or elevated prolactin levels. - Ultrasound
An ultrasound of the ovaries is another common test used in diagnosing PCOS. During this procedure, your OBGYN uses sound waves to create images of your ovaries. In PCOS, the ovaries often have a characteristic appearance, with multiple small cysts (fluid-filled sacs). While the presence of ovarian cysts is a key feature, not all women with PCOS have visible cysts on an ultrasound, which is why other tests are also necessary for a conclusive diagnosis. - Ruling Out Other Conditions
Because the symptoms of PCOS can overlap with other disorders, your doctor will work to rule out other potential causes. For example, conditions like thyroid disorders, adrenal gland disorders, or other hormonal imbalances may present similar symptoms. To ensure an accurate diagnosis, your doctor may suggest additional testing or refer you to a specialist if needed.
Treatment Plans for Symptom Management
Polycystic Ovary Syndrome (PCOS) is a condition that presents differently in every woman. Your OBGYN understands this and designs treatment plans tailored to your unique symptoms, lifestyle, and long-term health goals. These plans aim to manage symptoms, prevent complications, and improve your overall quality of life. Below are the key components of a comprehensive treatment plan:
Lifestyle Guidance
Lifestyle changes are a critical part of managing PCOS symptoms, especially for addressing insulin resistance and weight-related challenges. Your OBGYN can offer practical guidance on adopting a balanced diet rich in whole grains, lean proteins, and healthy fats while minimizing processed foods and added sugars.
Exercise recommendations may also form a key part of your plan, focusing on activities that improve insulin sensitivity and support weight management, such as aerobic exercise and strength training. Additionally, managing stress through techniques like mindfulness, yoga, or counseling can help regulate cortisol levels, which often impact PCOS symptoms.
Medication Management
When symptoms persist despite lifestyle changes and hormonal therapy, your doctor may introduce medications to target specific challenges. For instance:
- Metformin: Commonly prescribed to improve insulin sensitivity and lower blood sugar levels, metformin can also support weight loss and regulate menstrual cycles.
- Ovulation-Inducing Medications: For women experiencing infertility, drugs like clomiphene or letrozole can stimulate ovulation and enhance the chances of conception.
- Anti-Androgen Medications: These may be recommended to reduce symptoms like excessive hair growth or male-pattern hair thinning caused by high androgen levels.
Each medication is chosen based on your individual needs and health profile. Regular follow-ups with your specialist ensure that the treatment remains effective and adjusts to your evolving health goals.
Addressing Fertility Concerns
PCOS is one of the leading causes of infertility, but that doesn’t mean parenthood is out of reach. Your OBGYN offers help to support your reproductive journey, including:
- Ovulation Induction
Medications like clomiphene citrate or letrozole can stimulate ovulation, increasing your chances of conception. - Assisted Reproductive Technologies (ART)
For more complex cases, treatments such as in vitro fertilization (IVF) may be recommended. - Tracking Ovulation Patterns
They can guide you in using ovulation kits or recommend advanced tracking methods to optimize timing for conception.
By addressing hormonal imbalances and providing fertility-focused care, your OBGYN ensures you have the best chance of achieving your family planning goals.
Emotional and Mental Health Support
The hormonal imbalances associated with PCOS are often linked to heightened stress, anxiety, and even depression. For example, the unpredictability of symptoms like irregular periods, weight changes, or acne can lead to frustration, diminished self-confidence, and social withdrawal. Stress, in turn, exacerbates these symptoms, creating a challenging cycle that can feel overwhelming.
Your gynecologist recognizes this intricate connection between PCOS and mental health. They understand that managing the emotional toll is just as important as addressing the physical aspects of the condition. Here’s how they can help provide much-needed emotional and mental health support:
- Providing a Supportive Environment
They listen to your worries, validate your experiences, and offer solutions to alleviate emotional stress. - Referrals to Specialists
If needed, your doctor can connect you with therapists, dietitians, or support groups specializing in PCOS. - Encouraging Holistic Wellness
They emphasize the importance of mental health alongside physical health, ensuring you receive comprehensive care.
When to Seek OBGYN Care for PCOS
When it comes to your health, you deserve doctors who truly care about you—not just your symptoms. At Atlanta Obstetrics and Gynecology Specialists, we’re here to offer more than medical expertise. We’re here to listen, to support, and to help you take control of your health. Whether it’s managing conditions like PCOS, finding relief during menopause, or understanding irregular cycles, our team works with you to create care plans that fit your life.
Not sure if it’s time to book a visit? If you’ve been dealing with changes in your period, ongoing pelvic discomfort, struggles with fertility, or even just a sense that something isn’t quite right, it’s worth reaching out. These are all signs your body might need extra attention, and having a trusted gynecologist can make all the difference in finding clarity and peace of mind.
Ready to put yourself first? Schedule your consultation with Atlanta Obstetrics and Gynecology Specialists today. Let us be the team you turn to for answers, solutions, and the care you deserve.